What is cell stress, why is it important?
“Any change in the cellular environment with the potential to damage cellular components effectively induces cell stress.
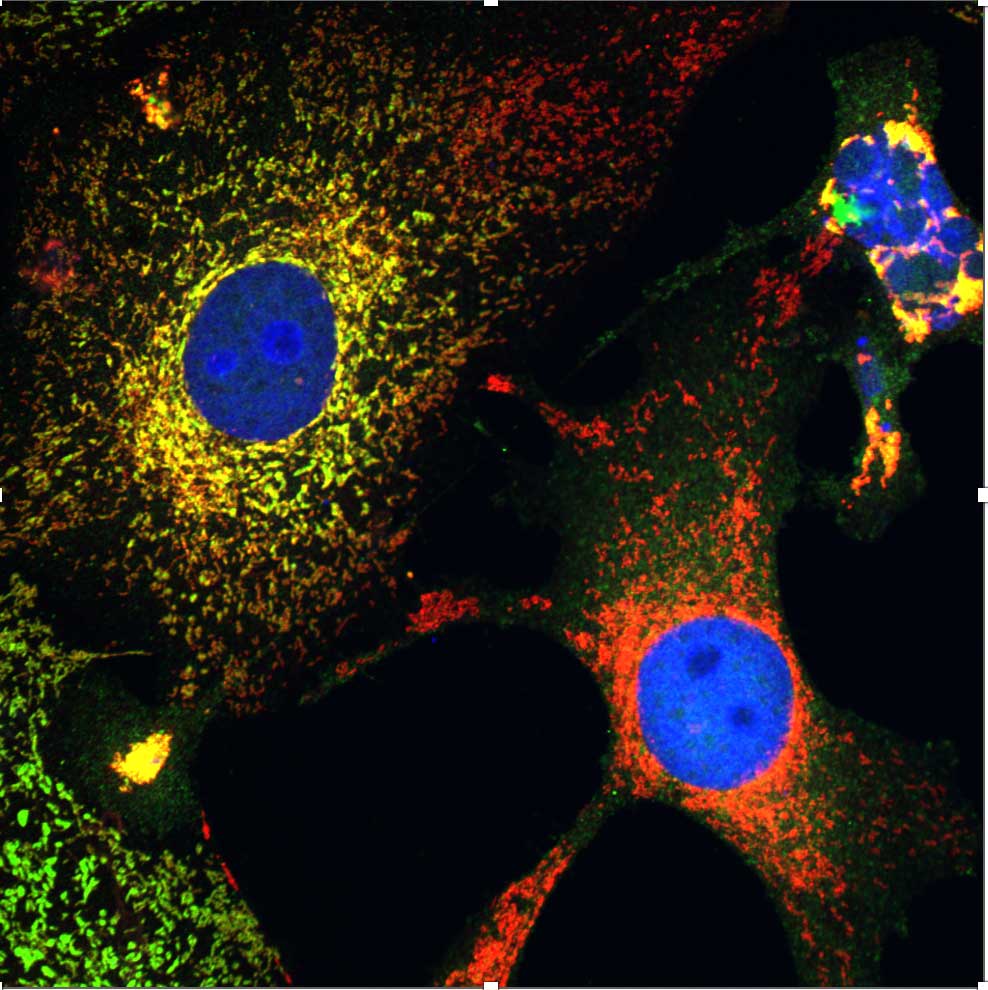
Cells experience different kinds of stress. Factors such as elevated body temperature, infection, exposure to toxins, such as excessive alcohol consumption, or intense physical activity during sports can all produce cellular stress. The body can also experience stress due to undernutrition, entering starvation mode, or due to overnutrition in cases such as type 2 diabetes. Such conditions may cause long term inflammation, which is a consequence of cell stress.
Tumours are another example of a situation associated with tissue stress. The development of a tumour indicates that cells are growing in the wrong place. As a lump forms, the lack of a normal vasculature leads to insufficient blood flow, nutrients and oxygen, with the result that cells of the tumor are in a state of constant stress and starvation, which can trigger inflammation. Unfortunately, an inflammatory response is often very beneficial for the tumor and can prevent tumors from being eradicated by the immune system.
Another example is when a patient undergoes chemotherapy. Not all of the cells of the tumour die after a single treatment with a chemotherapeutic drug. Usually several months of treatment are needed for the drug to achieve the desired outcome. However, with each cycle of chemotherapy cells of the tumor are repeatedly exposed to the drug and are damaged but not killed – in other words, they experience stress, which again provokes inflammation that can benefit tumors.
Several years ago, when we were treating cells with a chemotherapeutic drug called Taxol, which is given to millions of women every year to treat breast cancer and ovarian cancer, we realized that in many situations Taxol was not killing the cells but was causing tissue stress, which in turn induced an inflammatory reaction; but this type of stress-induced inflammation is very poorly understood."
What is the link with inflammation?
“Inflammation occurs when there is a trigger that disturbs normal tissue function and this elicits a response from the immune system resulting in the production of a battery of immune messenger proteins – which is called ‘’an inflammatory response’’. There are two major triggers of inflammation – infection and tissue damage.
Inflammatory reactions manifest in the initial phase of an infection or after a tissue damage, such as a twisted ankle. They are characterized by classic signs such as swelling, redness, heat and pain. Researchers are well aware of these responses, and drugs have been developed to target these types of inflammation.
However, inflammation presents in another scenario as well - where cells do not die but experience stress. Our primary research goal is to identify the pathways and sensors responsible for driving inflammation in scenarios where cells do not die but experience stress.”
What is a significant finding of your research so far?
"For over a decade, Interleukin 37 (or IL-37) was believed to be a molecule capable of switching off or suppressing inflammation, rather than driving it. Our recent research revealed that IL-37 could, in fact, play a role in driving inflammation. When cells are stressed or injured, they release cytokines and interleukins that switch on different arms of the immune system. IL-37 is a member of the IL-1 family, a group of cytokines often referred to as ‘danger signals’. When cells get damaged, they release IL-1 family members to initiate inflammation.
However, if IL-37 is modified in the right way it can promote inflammation, which was unexpected. Many interleukins, particularly within the IL-1 family, are initially produced as inactive and disarmed version of themselves and we found that IL-37 is activated by proteases released from certain white blood cells called neutrophils. This finding marks a step forward in understanding how IL-37 may contribute to inflammation. ‘’
What are your upcoming research plans?
‘’Something I am particularly excited about at the moment is understanding how oncogenes can drive inflammation. Oncogenes are mutated forms of genes that are commonly found in many cancers. These are molecules that when switched on, drive cancer and promote inflammation. This type of inflammation benefits the tumour. Inflammation consists of two major components: an immune response that expels the infectious agent that entered the body (in the case of infection), and an immune response that coordinates tissue repair after an injury; called a wound-healing response.
During wound-healing, the body produces molecules that encourage cell division, trigger the growth of new blood vessels and patch up the wound. Tumours really like such molecules and try to elicit the wound healing functions of the immune system because that is how they grow. Yet, how exactly tumors initiate this ‘wound-healing’ type of inflammation is still obscure. What we do know is that upon diagnosis, tumour cells are almost always infiltrated with a lot of immune cells. When we grow a tumour in a mouse in the lab, as much as 50% of the weight of the tumour can be the immune system of the mouse.
The same applies to human tumours, and the problem is that the body sees the tumour as a wound and the immune cells effectively nurture it instead of killing it. Tumour growth seems to be also driven by stress. That is a scenario we are very interested in – when oncogenes get activated and elicit a stress-induced inflammatory response from the tumour. We really don’t know how oncogenes promote inflammation and release of cytokines into the tumor microenvironment. This is a major focus of our work at present.”
How do you envision your research making a meaningful impact?
"The significance of our research lies in its clinical relevance to various health-related issues, such as cancer, obesity, neurodegenerative diseases, and other chronic conditions. The hope is to understand the pathways driving cell stress-associated inflammation, with the intention of developing targeted interventions to suppress such inflammation and improve treatment outcomes in these diseases.
Another main focus of our research involves understanding the inflammatory response to chemotherapy. Often, this response inadvertently benefits the tumour, working against the objective of the chemotherapy. Consequently, our aim is to find a way of effectively switching off this inflammatory response to enhance the overall effectiveness of chemotherapy. This can be achieved through the development of new drugs or by combining existing anti-inflammatory agents with existing chemotherapeutic drugs.”
What challenges do you find yourself grappling with in your work?
"One of the hardest aspects of our career involves securing funding. The success rate for the majority of grant applications is less than 10 percent. To put it into perspective, imagine successfully running a restaurant or other business for 20 years, and every few years you must reapply for funding to keep your business going with a mere 10 percent chance of success. This is the reality we confront - it's incredibly challenging to sustain a lab in the current research landscape. The significance of ERC funding cannot be overstated. It has served as a lifeline for many labs across Europe. Basic and fundamental research, which is the seed corn of the whole research ecosystem, has been consistently underfunded since the last global economic downturn, and the recovery has been slow. The presence of the ERC championing basic research has been crucial in navigating these challenging circumstances.”
Biography
Seamus Martin is one of the most highly cited scientists in the field of immunology. He is specialised in programmed cell death (apoptosis) which is vital for the development and the function of the immune system. In 2015 he received Ireland’s highest scientific excellence award, The RDS Irish Times Boyle Medal. Among other organizations he is a member of the Royal Irish Academy, the European Molecular Biology Organisation, Academia Europaea, has published several immunology textbooks and is editor-in-chief of The FEBS journal (a respected life sciences journal). He is also the former president of the European Cell Death Organization.





